

- Call 908 543 4390
- Email
- Dr.Joni Redlich PT,DPT


Spinal muscular atrophy (SMA) is a genetic disease that affects the central nervous system, peripheral nervous system, and voluntary muscle movement (skeletal muscle). A majority of nerve cells that control muscles are located in the spinal cord. SMA primarily affects muscles, because they don’t receive signals from specific nerve cells, called motor neurons. When muscles aren’t stimulated by nerve cells, they get smaller or atrophy. Because SMA involves the loss of nerve cells called motor neurons in the spinal cord, it is classified as a motor neuron disease.
Degree of motor function decrease is roughly correlated to the age at which SMA symptoms start. Generally, kids who have symptoms at birth or in infancy usually have the lowest level of functioning (type 1). As a rule, later-onset SMA with a less severe course (types 2 and 3, and in teens or adults, type 4) corresponds with progressively higher levels of motor function.
Chromosome 5 SMA is caused by a deficiency of a motor neuron protein called SMN, for “survival of motor neurons”, which appears necessary for normal motor neuron function. SMN has a crucial role for gene expression in motor neurons.

The scope of SMA symptoms are broad, and symptoms range from mild to severe. Typically the “proximal” muscles (closer to the center of the body) are the most affected in the body. SMN-related SMA presents with weakness of the voluntary muscles as a primary symptom and often include shoulders, hips, thighs, and upper back. Lower limbs seem to be more than upper limbs, and there is a decrease in deep tendon reflexes. If the muscles used for breathing or swallowing are impacted, there may be complications with those functions. Similarly, back muscles weakening may result in development of spinal curvatures.
Recently, there have been exciting treatments for various types of SMA that have been complete game changers for individuals who have the disease. Current research strategies have focused on increasing the body’s production of the SMN protein that’s lacking in the chromosome 5-related forms of SMA. Methods include approaches to increase motor neuron survival in adverse circumstances.
The Food and Drug Administration (FDA) approved Spinraza (nusinersen) for the treatment of SMA, on Dec. 23, 2016. Spinraza is designed to treat the underlying defect in SMA, meaning it potentially might be effective at slowing, stopping, or possibly reversing the symptoms of SMA.
In May 2019, the FDA approved Zolgensma (onasemnogene abeparvovac-xioi), which represents the first gene-replacement therapy for a neuromuscular disease. Zolgensma is a one-time intravenous infusion, and is used to treat pediatric patients younger than 2 years of age with SMA, who exhibit bi-allelic mutations in the SMN1 gene. This includes those who are presymptomatic at diagnosis. Read more information at: FDA Approves AveXis’ Zolgensma for Treatment of Spinal Muscular Atrophy in Pediatric Patients.
Additionally, the FDA approved risdiplam (brand name Evrysdi) in August 2020, for the treatment of SMA in adults and children two months of age or older. It is an oral medication that functions to raise SMN protein levels, by boosting production from the SMN2 “backup” gene.
For a detailed and simple-to understand overview of SMA, visit the Muscular Dystrophy Association website for the SMA fact sheet at:
https://www.mda.org/sites/default/files/2020/11/MDA_SMA_Fact_Sheet_Nov_2020.pdf
Currently, one of the best known people with SMA is Shane Burcaw. Shane has been affected by SMA most of his life, yet it doesn’t define him fully or keep him from living a productive life as a disability advocate, speaker and author. Together with his wife, Hannah, they run a popular YouTube channel ,“Squirmy and Grubs” and share their relationship story with the world, with the hope to change the way society thinks about disability.
The link below is a video on the channel where Shane talks about his diagnosis and early life. It also showcases the amazing relationship he and his wife share.

The CDC put out new milestone guidance for families and crawling was removed as a milestone. This decision led to a lot of uproar in the pediatric physical therapy and occupational therapy world and a lot of confusion for parents! Let’s have a conversation in this blog post about crawling and whether it is still important for us to consider.
First off, let’s consider the guidelines put out to parents and healthcare professionals. The developmental monitoring guidance, which is designed for parents to have a quick way to see if their child’s development is on track, no longer includes crawling as a milestone.
This does NOT change child development, developmental screening, or developmental evaluations. Developmental screenings are recommended to be done at 9, 18, and 30 months of age. Additionally, Autism Screening is recommended at 18 and 24 months of age. Any concerns about a child’s development will lead to a developmental evaluation, which looks more in depth at a child’s development.
Developmental screenings and evaluations will continue to include crawling as a milestone. Given that, we can include that crawling continues to be a milestone and one that is important to address.

In many ways crawling represents freedom. Crawling is usually the first time a baby can actively explore their environment, versus someone having to carry them from point A to point B. Babies also gain a sense of independence from their parent or caregiver, as they move away from them and then move back.
When babies bear weight on their arms, they develop shoulder stability and they develop the arches of the hands, which helps later on with handwriting and fine motor skills. Crawling also helps develop vision skills and gives babies important sensory feedback, from stimulating the vestibular system while moving in space, gives information to the touch receptors on the hands, legs and feet, and gives proprioceptive information from the joints and muscles. This sensory feedback helps babies develop spatial awareness, or the sense of where their body is in space.
Finally, crawling helps develop core stability and coordination, because you’re using your opposite arm and leg at the same time, along with moving in a rhythmic manner.
All of these components work together as the baby learns to control their bodies against gravity at this new level.

The most important thing parents that do to support their babies development is to have lots of floor time, without the use of supports, so that baby can explore.
Babies need to move against gravity, and see, by trial and error, when I reach for that toy, what happens? A lot of times they start moving by a happy accident, like they lean one way to get something and they roll over. If they don’t have those opportunities, those happy accidents can’t happen.
When the baby is on the floor, encourage them to move by putting toys slightly out of reach. As parents, having the patience to let them go through that trial and error process and not jump in can be so hard, and sometimes even I have to sit on my own hands.
The transitions babies do over and over again during play, moving from sitting to belly and back to sitting, from sitting to hands and knees to sitting again, is what gets their little bodies truly ready for crawling. They move in and out of positions, getting their core muscles primed to support them on hands and knees.

Many babies will crawl in a typical all fours pattern, but there are so many variations too. Some babies will first commando or army crawl before getting up on hands and knees. This is where we often see lots of different variations and asymmetries. Some babies will do lot of pulling with their arms and some will always push off with the same leg. I generally tell parents not to worry about funny looking army crawl patterns. It will work itself out when the babies are on hands and knees crawling and moving in a much more symmetrical and synchronized way.
Some babies will bear crawl, where the legs are kept straight. This often happens when the baby is avoiding hard floors! As long as you’re seeing lots of variety of movement patterns during play, this isn’t concerning.
Crab crawl: Baby moves with either one or both legs tucked under. This is another common variation. Its often due to asymmetries in the pelvis and hips, but it can also just be a normal variation.
Bottom scoot: Baby uses hands to push across the floor while sitting upright on their bottom. Some babies don’t go onto hands and knees at all and will get around on their bottoms. If baby is choosing this method of mobility, keep an eye out for how they are figuring out how to pull up to standing so that they are able to get to the next stages of development on the road to walking. My favorite activity to introduce to bottom scooters is climbing up the stairs- you can’t pull that off with a bottom scoot!
Crawling backwards: many babies will crawl backwards before figuring out how to crawl forwards; if you see your baby crawling backwards, just enjoy the process and watch them problem solve and figure out how to change directions; they’re almost there!

Babies will learn to crawl on hands and knees between 8-10 months of age. Like every milestone baby works towards, there are many small steps that add up to the big achievement of the milestone. If a baby is able to do all the steps up to crawling, such as moving from sitting to hands and knees and rocking on hands and knees, they’re on their way.
Some signs baby may need some help with their gross motor development:
At Kid PT we offer developmental screenings to local families who have questions or concerns about their children’s development. I tell parents that at that screening you will either get peace of mind that there aren’t any concerns or they’ll get recommendations as to how to help their child and support their development. Its a win-win!
To schedule a Developmental Screening, call/text us at 908-543-4390 or email info@kidpt.com.
What happens when your child is ill?
Have you ever thought you were going crazy when it came to your kids? Sure, we all get stressed out by the demands parenting requires of us whether they be mundane, daily happenings (“No you can’t have another cookie!”, “Stop teasing your brother!”) or extreme, unlikely circumstances (Hello pandemic-looking at you!)
But, what if there was something wrong with your child, (who also happens to have neurodevelopmental delays or another neurodivergent diagnosis) and no experts had any answers for you? What if you took your kiddo to all the “BEST” doctors out there and they either had no answers, their diagnosis conflicted with one another, or worst of all, they just didn’t believe your child had a problem?
Misdiagnosis happens.
I am here to tell you that it happens. And when it is your child who is struggling and suffering, it is exquisitely painful. You feel like you are living in a nightmare that you simply cannot wake from and that somehow, those around you are seeing a distorted view of reality. A 2019 article* states that, “the mindset that young children are rarely seriously ill is one of the main reasons that they are more likely to be misdiagnosed than adults are. That’s on top of all of the ways that approximately 10 percent of American adults are misdiagnosed every year. When doctors and nurses expect to see a healthy child with a common short-lived illness, they may miss the uncommon ones.”
The article goes on to list the main reasons for children receiving a diagnosis that’s wrong or delayed:
Experts may give you the brush off.
However, there are cases where a parent’s concerns are dismissed, as I was when my daughter presented with a long, puzzling, seemingly unrelated laundry list of symptoms that spanned years, nearly a decade by the time a diagnosis was finally rendered. During that time period, I was given advice from some well-meaning individuals who said things like:
Did any of this help my daughter get better or me find answers? That would be a resounding no. Oh, and by the way, that last piece of “advice” above was given to me, in front of my child, by a supposedly well-respected doctor. He dismissed all the hundreds of pages of tests, scans, medical records and prior diagnosis, didn’t help my daughter, and charged for it!
So what DO YOU DO? You don’t give up- you trust your gut! Parents know their children best and what their “normal” looks like, even if it doesn’t match the textbook image. Remember to believe in yourself and your ability to help your child. Make a bulleted list of every symptom, even if it does not seem totally related, and the date the symptom started. Research the heck out of your child’s symptoms and any test results you have, using the best and most trusted resources you can find. Become well acquainted with clinical research papers, societies for various branches of disease types ( think brain, stomach, nervous system, etc.) Join an online group for other parents who may be seeking answers for their child or who may have information to share.
The Society to Improve Diagnosis in Medicine says not to get overwhelmed by the risks of misdiagnosis. Rather, recognize there are a few key things to do, to assist in getting an accurate and (hopefully) prompt diagnosis. These tips also help if your child is in the middle of a diagnostic journey today.
In closing, you, as a parent, are the most trusted authority on your child. If you feel that something is wrong with your child and it is not getting resolved, don’t be afraid to speak up. Your child and your family deserve answers and the best possible care. Be brave and know that what your GUT is telling you, may be right. (If you have a question for Melanie (author/Kid PT Marketing) email her at info@kidpt.com)
*References

I have to admit, I’m not the most coordinated person. You may have noticed the same about yourself or your child.
The big question parents often ask me is whether their child is on the clumsy end or is there another explanation for it.
The biggest question to ask yourself is whether your child’s clumsiness is impacting their everyday life. Is it making them a wallflower on the playground? Is it making it difficult to make it through a meal without spilling or dropping something? Is the child tripping frequently or bumping into things?
Partially because clumsiness has been the butt of so many jokes in media, its often not taken seriously. The truth is that clumsiness doesn’t naturally improve and can have a really big impact on a child’s confidence and self-esteem.
Plus, therapy can help! So if there’s a big problem impacting a child’s everyday life that is making them feel bad and we have the power to improve it, we can’t overlook it!
Let’s take a look at 2 different people with Developmental Coordination Disorder (DCD), how it impacts their lives, and then we can talk more about how to know when to seek help.
Jane is a very warm and friendly seven-year-old girl diagnosed with developmental coordination disorder and dyspraxia. She has never had success with academic, gross motor or fine motor activities, and prefers to talk her way out of challenges. Talking she is good at, but only with adults. She has struggled to make and keep friends.
Jane started a PT program at Kid PT and after two months of participating in a program working on her visual-motor and rhythmic movement skills, her mom reported that not only was she moving better, but she was having so much more success socially.. Mom said, “I can imagine that if you can’t keep up with the kids on the playground, that’s going to affect your confidence playing with the other kids.”
Mom’s observation was so true and impacts so many children everyday. Our innate sense of rhythm runs in the background of everything we do. It affects how we interact with others and how we multitask emptying a backpack at school while saying hello to a friend while smiling and remembering everything you need for the day. The consistent and reliable rhythm of our brain and body supports all of these seemingly mundane tasks that can be overwhelming if you have to think about them every step of the way!
After 17 years of struggling with his body to get through daily life, Jimmy came to Kid PT.
For years, Jimmy’s pediatrician told his mom that he would grow out of his clumsiness and to just keep him active. He played rec soccer and baseball, but he was always lagging behind and by the time he entered middle school he just gave up on sports altogether. He was a talented artist and loved video games, so he kept himself very busy with those activities.
Jimmy’s mental health was suffering though and he was struggling to get enough energy to get through each day. His mom had a friend that said to come to Kid PT and see if we could help.
During his evaluation, I identified many sensory and motor deficits that were greatly impacting all of his movement skills. His vestibular function (inner ear) was impaired, particularly the vestibular ocular reflex, which keeps vision steady as we move through space. His vision was working too hard trying to make up for vestibular impairments, so his balance was decreased at night when vision couldn’t be relied on as much.
He also had postural asymmetries that he was likely relying on for years that were causing musculoskeletal issues, in addition to affecting body awareness. His movement system had never gone on autopilot. He had to focus so much on moving his body to get through his daily routines, that it was zapping up so much of his energy, leaving him fatigued and frustrated.
Understanding the building blocks of development of the movement system for a teen, who has only experienced failure with the practice, practice, practice approach, can change one’s perspective dramatically.
Instead of blaming yourself for not trying harder, you can own your challenges, empower your strengths, and begin to move forward. Awareness of his challenges didn’t change his body immediately, but it did change his perception of himself.
Children with Developmental Coordination Disorder (DCD) are not simply clumsy. DCD is a motor skills disorder that affects approximately five to six percent of all school-aged children. DCD has been described in many ways over the years, including dyspraxia, minimal brain dysfunction, and clumsy child syndrome. The medical community has chosen to use the term DCD as the preferred diagnostic term. DCD occurs when a delay in the development of motor skills, or difficulty coordinating movements, results in a child being unable to perform common everyday tasks. They often have difficulty keeping up with their peers during gross motor play, have frequent falls, and have a hard time doing daily skills, such as zipping and tying shoe laces.
The biggest challenge is often with learning a new movement-based skill, which is a challenge that is experienced throughout childhood. These children are often labeled as lazy (read more about how NOT lazy these kids are here!). They’re often told that if they would just try harder they could do it. In the past, it was often assumed that children would outgrow these challenges, but research has demonstrated that children with coordination problems do not simply outgrow these problems. In fact, these children are at greater risk for being sedentary and less healthy as adults than their peers. These children are also at greater risk for mental health problems. We cannot risk overlooking the struggles of these children. There is too much at risk for their futures!
Children with DCD are constant victims of imperfect practice. These children blend in with their peers well and are often not even diagnosed. Goal-oriented methods help with the practice component, but this is not enough. Life will constantly present new skills, so this creates a constant challenge, especially throughout childhood. In addition to working towards specific skills, we can work on developing a child’s building blocks of movement in order to also “teach the child how to fish.” Building the foundations of movement, rather than just teaching gross or fine motor splinter skills, improves the child’s learning abilities and decreases their reliance on others.
Children with DCD often have low tone, as well. Due to the low tone, it is generally assumed that these children are flexible everywhere. However, when you look closely at their core, the opposite is often discovered. Children with low tone typically don’t develop sufficient three-dimensional control in their core. Without the development of core control, asymmetries often remain and limit the development of core control. Often parents will tell us their kids will just randomly fall out of their seats in school (learn more about why here!).
Children with coordination disorders can vary in their vestibular responses. The vestibular system can be underactive, limiting the child’s ability to develop a strong sense of where they are in space, or the vestibular system can be oversensitive, leading to fear of movement. Low tone and hypermobility can lead to less information going from the joints and muscles (proprioception) and traveling to the brain to tell us where we are in space. Commonly, the visual system will work hard to make up for less teammates in the balance team.
Many children with coordination disorders will have difficulty getting their bodies stacked up with good alignment in order to turn their power on. These kids will often hold their bodies in an alignment that feeds into chest breathing, with their chest shifted up and their back appearing to be arched. This position and breathing pattern feeds into the child’s fight-or-flight system, or sympathetic nervous system, and gives them less ability to use their calming parasympathetic nervous system.
Children with coordination disorders struggle to put all of the pieces of their movement skills and sensory feedback together to be able to combine it with timing, sequencing, and multitasking. Being able to do this is demanded from a student, even in kindergarten! Because of this, beginning school is often the turning point for parents to seek out extra help for their child.
We move through daily life without consciously thinking about how we are moving our bodies. We can walk while daydreaming without bumping into a street sign, and we can sit in a chair without falling off while reading and writing. This may sound natural for many of us, but children with postural deficits use excessive energy, attention, and focus to fulfill all of the expectations they face each day. When our gears are synchronized, movement is automatic and children can focus on higher level skills, whether it is moving through the classroom without bumping into things or learning algebra. Filling in or strengthening these missing building blocks to develop a child’s sensory-motor system can build automaticity in order to multitask and to free the child up for higher cognitive skills. That’s where we can help!
Children with coordination disorders are often called lazy and told they’re not meeting their potential. People assume things will get better as the child gets older and that these are delays that will “catch up.” In the meantime, the child struggles with their self-worth, self-esteem, and mental health. As we said before, research supports that children do not grow out of these struggles, and that children with coordination challenges are typically more sedentary adults with increased risk of cardiovascular and mental health problems.
Supporting a child’s ability to learn the skills they need in daily life is important, but we cannot fall into the work harder and try harder pit, without also working towards long-lasting change. We can help these children fill in those missing and weakened foundational skills. There are so many ways we can help these children meet their personal potential and protect their mental health, all at the same time. They are working so hard, day in and day out- let’s acknowledge that, support their efforts, and improve their building blocks so that they are building their houses with the strongest foundation as can be.

If you see your child is working harder than other kids to get through their daily activities, don’t wait to look for help. You also don’t need an official diagnosis to get help. Reach out to us at KidPT and come in for a Discovery Visit. We will listen to your concerns, do a screening of your child and their movement skills, and help you make a plan. We’re here for you!
References
Hi all! We know June for being the last month of school and the month where summer fun begins, BUT did you know June is also Scoliosis Awareness Month? Yes! June is the month where we highlight Scoliosis, a diagnosis that affects so many kiddos (and adultos☺️) across the world. So, for Scoliosis Awareness Month, we wanted to bring you all some information about Scoliosis, what it is, and how Physical Therapy can help!
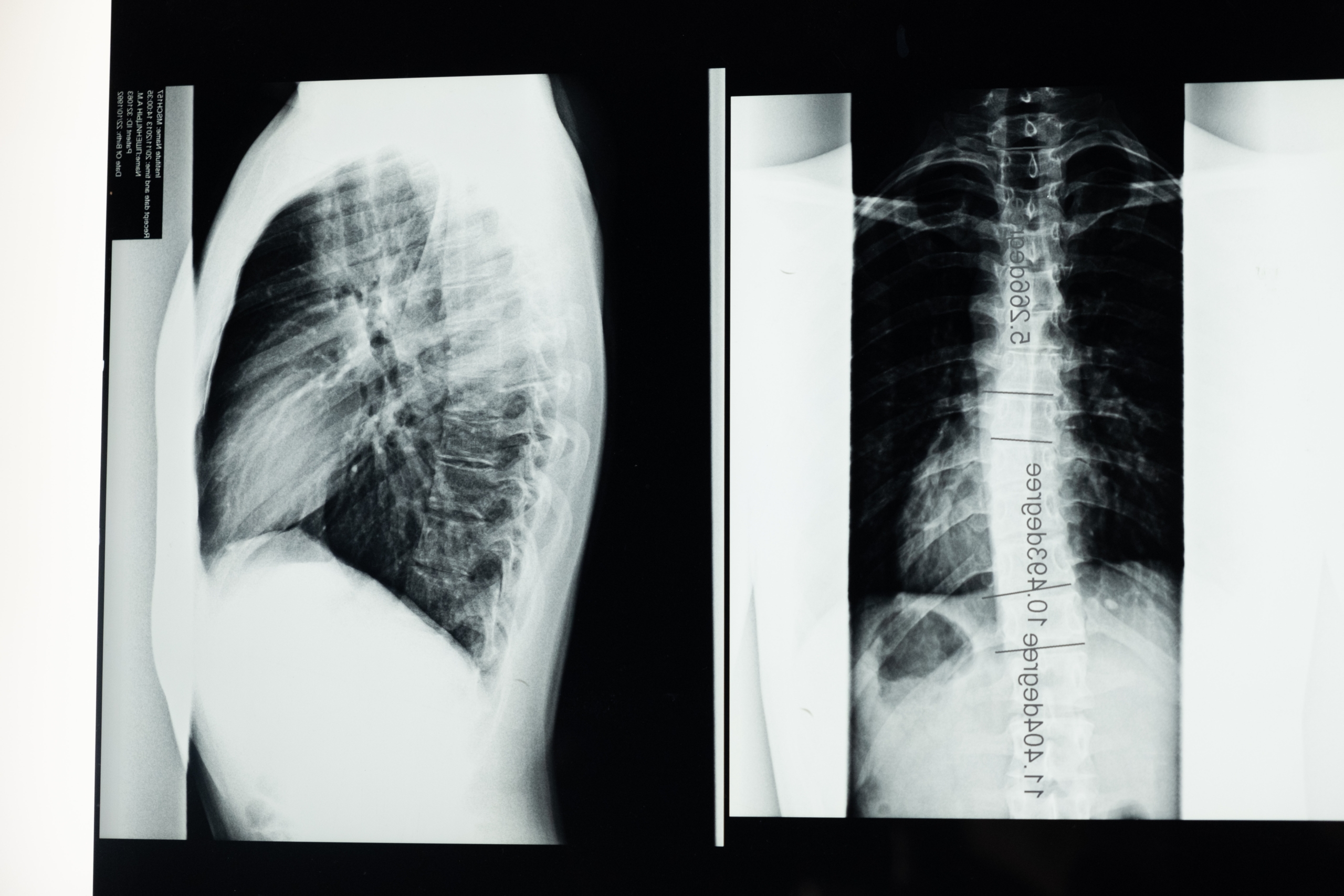 Scoliosis is a diagnosis that involves a curvature of the spine, the bones that run along the middle of your back. If a child is affected with scoliosis, as they grow, their spine will begin to curve in either the cervical, thoracic, or lumbar spinal regions, aka the neck, upper back and lower back regions. Changes in the spine’s natural anatomy create imbalances in the body that may cause your child’s shoulders, shoulder blades, hips, or ribs to look unlevel or uneven. It may also cause their spine to appear curved when bending forward, may affect their overall mobility, and may create back pain later in life if left untreated. If a child’s scoliosis is very severe, it can also affect the shape and growth of their internal organs, like the lungs or the heart.
Scoliosis is a diagnosis that involves a curvature of the spine, the bones that run along the middle of your back. If a child is affected with scoliosis, as they grow, their spine will begin to curve in either the cervical, thoracic, or lumbar spinal regions, aka the neck, upper back and lower back regions. Changes in the spine’s natural anatomy create imbalances in the body that may cause your child’s shoulders, shoulder blades, hips, or ribs to look unlevel or uneven. It may also cause their spine to appear curved when bending forward, may affect their overall mobility, and may create back pain later in life if left untreated. If a child’s scoliosis is very severe, it can also affect the shape and growth of their internal organs, like the lungs or the heart.
There are four different types of scoliosis: idiopathic, neuromuscular, congenital and degenerative. Degenerative scoliosis is often diagnosed above the age of 65 due to normal wear and tear on the spine and surrounding joints. Congenital scoliosis occurs as a result of spinal or rib deformities present at birth. Neuromuscular scoliosis can occur when a child has a neuromuscular condition, like cerebral palsy or muscular dystrophy. With Neuromuscular scoliosis, as the child grows, their muscles pull on their bones as they move and continue to participate in developmentally appropriate activities. When a child has a neuromuscular condition, they might not be moving with similar movement patterns or frequency to a child that is developing typically. This means that their muscles are not pulling the same way on their bones as a typically developing child’s muscles are, and this can cause their bones to grow abnormally, creating a potential for scoliosis.
Adolescent Idiopathic Scoliosis is the most common form. It can be a confusing diagnosis for families to receive because it is often unknown as to why the spinal scoliosis is occurring in the first place. Medically, doctors will often recommend either a “watch and see” approach, monitoring the spinal curvature to see if it is progressing or staying the same. If a scoliotic curve is on the more severe side, or continues to worsen with time, doctors will often recommend bracing to try to prevent the curve from continuing to worsen or will recommend surgery to correct the curvature. Doctors will usually also recommend Physical Therapy, and that’s where we come in! BUT, you don’t need to wait- starting Physical Therapy at the first signs of scoliosis can prevent it from progressing in the first place!
What are some signs that you should ask your child’s pediatrician or a physical therapist about scoliosis? Take a look at your child from behind without a shirt on. Look at your child’s shoulders, shoulder blades, and hips. Compare the left and right sides looking for one side higher than the other. If you see any asymmetries between the two sides of the body, that is a sign to have it looked into by a medical professional.
In PT, we will work with you and your child as a team to help decrease any soft tissue and muscular tightness that may be pulling on your child’s spine while they are growing. We will also work with your child to improve their core strength so that as they continue to grow and improve their mobility, their body can better support itself to control and maintain their new, more-symmetrical posture. If they are having trouble holding a more symmetrical, stable posture while sitting at their desk in school, a physical therapist can also help improve your child’s postural endurance and offer solutions to help improve their sitting posture so that they can sit while supporting their body in class.
We understand that scoliosis can be a very scary diagnosis, especially when your doctor starts describing the ways it may affect them and about your treatment options. Through treating kiddos with mild to severe scoliosis, we have found that acting quickly and starting PT as soon as your child receives a diagnosis of scoliosis is the most effective way to help prevent future progression of their spinal curve. We are here to support you through the decision making process and to help provide therapy that will work to improve your child’s body through movement in a way that is friendly and fun!
If your child has just been diagnosed with scoliosis, or is being watched for scoliosis and you would like to be more proactive with their care, reach out to us with questions and to schedule a free Discovery Visit so that we can see if physical therapy here at KidPT is the right match for you and your child.
References: https://www.btetechnologies.com/therapyspark/4-types-of-scoliosis-and-their-interventions/

Happy Father’s Day to all of our amazing Kid PT Dads!
Dads know just how to bring a laugh and a giggle to the moment.
Check out these ideas to bring some movement fun to celebrate how much your kiddo loves you on Father’s Day!
First, hold each other’s hands. Can you lift one foot and hold it? Try taking turns closing your eyes and see if you can still both keep your balance. Add in singing a song together like the ABCs and see if you can balance all the way to Z.
Next, have Dad get into the Downward Dog position! How many times can the child crawl under, run around to the start, and climb under again! Let’s really challenge Dad with this one!
Finally, its time to fly! There are many fun ways to do this, from piggyback rides to holding the child and zooming around the house. My favorite way is for Dad to lie on his back his his hands and feet up. Dad puts his feet on the child’s belly, holds the child’s hands, and lifts them up! This is so much fun, just be careful. Be sure there is nothing nearby the child can fall on and only go as high as you can control.
What other movement adventures can you have today?
Did you go on a bike ride together, go on a hike or walk to the park?
Have a Happy Father’s Day!!!
The kids are getting out of school, the weather is getting VERY warm, and many families are looking for things to do! Many people are starting to think about backyard barbecues and other fun, family friendly activities as we picture our summers! Don’t forget to include some gross motor fun into your next backyard barbecue extravaganza. These activities below are sure to keep your kids moving and having a blast!

Sack races are so much fun and allow kids to jump, jump, jump to the finish line in a way that engages their competitive side and gets all of their energy going! Jumping with your legs together is a great way to work on coordination and strength while getting a little bit of that extra energy OUT! If you think this would be a fun idea, you can buy sacks for outdoor racing here:

Have all the children stand in a big circle, where they can all see each other! In a movement circle you can play fun games like “Pass the move” where every child does one move and then everyone repeats the move. These moves can be linked together to form a whole mini dance to keep kids moving and grooving in a funky way! In the circle, they can also move along to kids music specifically created for movement, like “Simon Says”, “The Hokey Pokey”, and “Animal Action”. Look for children’s movement songs on YouTube, Spotify, or other music Apps. There is also a whole YouTube channel of children’s movement songs through GoNoodle too, if your child loves silly characters! Here are a few links to some fun ones:
Animal action: https://www.youtube.com/watch?v=30ePPeUbwSs

For this one, have each child choose one item they want to put in their obstacle course (so that no one is touching the same items). Have them make up a specific rule for how to use their part of the obstacle course and have each child explain that rule to their friends. By the end of all the explanations and the building process, they will have created a full obstacle course as a team! This will help them use their creativity and collaboration skills before each of them jumps into action to move through their creation, helping them to work on strength and coordination too!

This old classic is great for working on jumping and hopping, and makes kids switch feet on every step, so it is also great for coordination. It can be set up with simple sidewalk chalk on a driveway or blacktop at the park. Jumping between numbers can be made even more fun and tricky if you ask the children to skip certain numbers, say their top ten favorite animals with every jump, or come up with their own wacky pattern for jumping through the squares.
Have fun out there everybody, keep moving, and enjoy the start to your SUMMER! Let us know @Kidpt on Instagram and @KidPTNJ on facebook or by emailing us at info@kidpt.com to tell us how these outdoor games worked out and if you want more fun ideas for how to keep your kids moving this summer!

There is so much nature and wonder to experience in a garden. Here in the KidPT garden, we invite your kids to participate in shoveling the soil, transferring dirt with a wheelbarrow, jumping over the rows of vegetables, imagining they are earthworms tilling the soil, shading the garden as nearby trees, and invading the garden as clever rabbits.

Have your child assume the wheelbarrow position by pushing up through their hands on the ground and have a sibling or friend hold them at their knees. The child on the ground will walk forward on their hands while the other child follows them supporting their lower body in the air. Then have them switch roles. If the child’s back is arched (aka the stomach is dipping downwards towards the floor and is lower than the chest and ankles), make it easier by holding them closer to their trunk until they can keep their back straight. Too easy? Hold the child further from the trunk and as close to the ankles as they will tolerate.
Line up pillows or rolled up towels on the ground and have your child jump over them. Have them name the row of vegetables that they are jumping over as they jump. Switch it up by having them jump sideways and backwards too.

Start in a standing position and have your child slowly lower their hands down to the ground in front of their feet. Then walk their hands forward as far as they can with their feet planted on the ground. Then walk their feet up towards their hands. Repeat as they squirm their way across the room.

Have your child stand on one leg and rest their other leg’s foot on their inner thigh. Once they gain their balance in this position, have them wave their arms in the wind just like a tree. Who can make a tree with the largest branches? Too hard? Instead, have your child place one foot on a step that is in front of them.
Set up the imaginary fence by extending a long piece of tape or string from one kitchen table leg to another ( or any stable surface) at about a foot height off the ground. Then have the kids take time to army crawl under the imaginary fence to the garden.
What are your family’s favorite garden activities and plants to grow?

May is Arthritis month! Why are we talking about Arthritis? Well, it’s not a diagnosis that only affects adults, it affects kids too. Juvenile Idiopathic Arthritis is a diagnosis that affects kids of many ages, both young kids and older teens too. Unfortunately, Juvenile Idiopathic Arthritis (JIA) is sometimes passed off as “growing pains” by some medical professionals when a child complains of joint pain. This is seen to happen more frequently with older children or young teens complaining of joint pain because at this time in their lives, they are going through large periods of growth and physical development. Sometimes it is just growing pains, but sometimes it might not be! We wanted to give parents and therapists a guide so that you can recognize when signs and symptoms of JIA might be present and know who to seek out for help if you think your child might be showing some signs and symptoms of JIA.
JIA (also known as Juvenile Rheumatoid Arthritis), causes joint stiffness and joint swelling, also known as inflammation. JIA affects one or more joints for at least 6 weeks or more in children who are 16 years old or younger. JIA is different from Adult Rheumatoid Arthritis, because symptoms can decrease or go away completely as they get older BUT it can affect how a child’s bones develop as they grow.
JIA is an autoimmune disease. An autoimmune disease can occur when the body’s immune system becomes overactive and begins to attack its own healthy tissue. In JIA, the primary tissues that are affected are bone and cartilage around the child’s joints. When this begins to happen, it can happen chronically or episodically. If a child’s JIA symptoms are chronic, they have them most to all of the time where as if they are episodic, they may go through flare ups where their symptoms get worse and then have periods where they have no symptoms at all.
Children with JIA primarily have symptoms related to their joints like swelling, stiffness, and pain. The joints that are most commonly affected are the knees, hands, feet, ankles, shoulders, and elbows, but the spine and hips can also be involved. Pain and swelling are often at their worst in the morning or after a nap. Children can also have decreased appetite, poor weight gain, slow growth, eye inflammation, and fatigue. In systemic JIA, children can also present with a high fever, rashing, and swollen lymph nodes. The tricky thing is that some of these symptoms can seem like other illnesses or health conditions so it is important to make sure your child is seen by their primary doctor and a rheumatologist for appropriate diagnosis.
Yes, They absolutely do! Physical Therapy is essential for kids with JIA to help preserve joint function and to help strengthen the body to better support the joints. When a child has JIA, strengthening has to be done carefully so to not overstress the joints, and PTs have the expertise to help guide you and your child away from activities and sports that may be harmful for your child’s joints and toward more helpful activities. In acute phases of JIA, when your child is exhibiting a flare up of their symptoms, PT helps to maintain their joint range of motion, prevents muscles from getting too weak, and helps protect their bones from getting weak too. When your child is not experiencing a flare up of pain and stiffness, PT will help improve your child’s gross motor skills, especially ones that may have been limited due to their pain and decreased range of motion, so that they play and move with more freedom and confidence. If a child has a more chronic form of JIA, physical therapy will also help to achieve new mobility goals while making sure to keep their pain levels low and to prevent increased swelling.
If your child has a diagnosis of JIA or if you think there is a possibility they may have JIA, talk to your child’s primary care doctor about whether or not they believe JIA is a possibility and what your next steps should be. If your child is experiencing joint pain, they may benefit from physical therapy for all the reasons discussed above and more. Our therapists at KidPT can help give you more information and can take a look at your child to see if physical therapy would be an appropriate next step to help their body grow and develop in the healthiest way possible!
If you want to learn more about the different types of JIA, the process for diagnosis for JIA, and more, click to read the article below:
References:

Happy Mother’s day to all our moms. Today we celebrate the unmatched and superhuman strength of mothers. Motherhood comes in many forms from biological to adoptive to a grandparent caregiver to legal guardian to working mom to stay at home mom to single mom to military mom and so much more.
Every mother is different and has their own strengths and weaknesses, but we want to applaud you and encourage you for all you do.
Raising a child is the most vulnerable, life-giving, exhausting, and worry-filled adventure we can go on. From the extreme highs to the devastating lows, it can feel indescribable. But our legacies are the children we love and support so that they can live a life of joy and meaning.
On this Mother’s Day we are celebrating a few of the many strengths of moms. Today is a day to just honor and acknowledge who you are day in and out. No need for tips, tricks, or advice today as you are enough, mom.
Emotional Strength
You deserve to be applauded for the emotional weight you carry in your home. It can be hard to be the emotional reservoir for an entire family. It can seem that you are always worrying about something as a mom whether it’s managing their schedule, academics, nutrition, health care, transportation, sleep, etc. Sometimes the constant thoughts and the emotional weight can take a toll on you and all you can do is just sit on the couch in mental exhaustion. This is no sign of weakness when you consider the strength and endurance it requires to constantly carry and nurture your family’s needs.
Physical strength
The physical strength needed to be a mother is nothing short of extraordinary. From the physical expense of carrying a child in the womb and the physical changes that your body undergoes while nurturing your baby’s life to the physical demands of carrying, bathing, cleaning, feeding your child and managing your household. Sleep often becomes a long lost friend from sleepless nights caring for your infant to catching up on “me time” or other tasks while the kids are in bed. There is nothing like the physical strength of a mother to overcome these hurdles in order to provide for the needs of herself and her family.
Resilience
Every day comes with its own journey, victories and disappointments. Parenting is a marathon and it may feel hard to see the progress of your parenting each day. Despite this, you push on and do your best to remain hopeful and engaged. It may seem the values you are trying to teach your children are not taking root and that your efforts are ineffective. But how sweet it tastes when you are awarded little glimpses of your children practicing strategies that you have been intentionally trying to instill in them, whether it’s noticing their kindness in how they treat others or signs of their developing bravery, emotional intelligence, and self regulation. You are resilient and your children will learn to be resilient through your example. Don’t underestimate the moments when you help them conquer their fears and how you make them feel heard and understood when they are struggling. It’s all too common for mothers to look around and convince themselves that everyone else is doing life better and that other mothers always do the right thing. It’s normal to have these feelings and doubts and to perceive that your world is in chaos. It is hard to figure out which route or philosophy to take with parenting and it is easy to feel overwhelmed. Despite this negative self talk, things are going better than you imagine and your kids are thriving from your strength and resilience.
From our families to yours, we hope this Mother’s Day you feel seen, affirmed, and loved.
